People living with a bleeding disorders know a thing or two about pain. Many with arthritis report having to wait until their body “loosens up” before they can begin their day. There’s also the pain you may feel after a particularly busy day when you’ve been on your feet, and that joint that always bothers you is “talking” to you more today than usual.
So how do you talk to your provider about how best to manage your personal pain experience? There are several tips and tools you can use.
First, pain is a personal experience that can be difficult for others to truly understand, so it is up to you to help your provider understand your pain experience. In doing so, you have a better chance of working as a team to best develop a good pain management program that will work for you.
Can you describe your pain? When you put it into words that others can relate to, it helps others to understand better. For example, when you say that the pain is “throbbing,” “sharp like a needle,” or “burning,” these descriptions better help others to visualize, relate to, and understand what it feels like. Does the pain move around, or does it stay in the same place all the time? Can you point to a specific spot where it hurts, or does it just seem to be the whole area?
You know what has worked or not worked for you in the past as you have made attempts to relieve your pain. Make a list. Talk about what medicines or treatments you have used that may or may not have made a difference. Why repeat a treatment that never really worked before? Making a list of what works and what doesn’t can help.
Quantifying your pain can provide additional information. You may be familiar with the pain rating scale of 0 being no pain, and 10 being the worst you could imagine. Sometimes it is hard to put a number to your pain, but it gives your provider a starting point. When treatments have been started, by using a number scale for pain, we can identify if it is improving or not. For example, if you rate your daily pain as 5 out of 10, then that suggests that you are living with a fair bit of pain every day. Most people can relate to that. Say you start a planned therapy, and as a result, your daily pain level is now 3 out of10. It’s better, but more importantly, it provides a framework of where you are and where you want to be. If the rating scale doesn’t work for you, think of a word list that can help, such as tolerable being the least amount of pain at one end, and excruciating being the most amount of pain at the other end. Some people find describing a percentage of improvement is helpful. “Using ice on my joint, helped decrease the pain by 50%.” Work with your provider to find the best rating system that works for you. Â 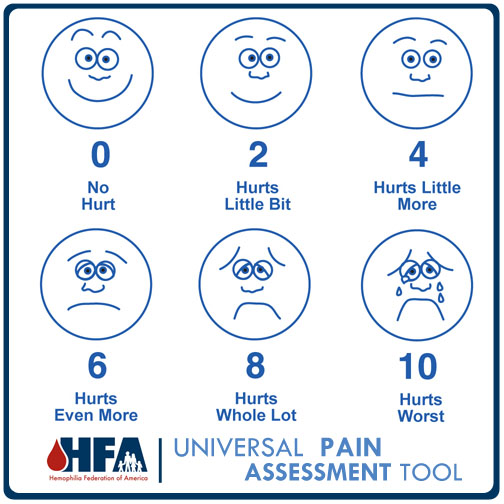
You should have a pain goal in mind. This doesn’t necessarily mean that you should be absolutely free of pain or 0 out of 10. That may not be possible, especially if you experience a level of pain every day. But, you should target a goal that is manageable. Another way of describing a measurable goal is to say, for example, “I want to be able to get dressed in the morning with 50% less pain than I am feeling now.” This provides a target to strive for and you can know when you have reached it. Â Â Â Â Â
It is also important to discuss what activities you do which make the pain better or worse. “I can walk 1 block just fine, but I just have too much knee pain when I try to go to the store to do some shopping.” This example provides information that your provider can relate to-how far you can go before it hurts. Keep in mind that even though you may be having pain in your joints that you think is hemophilia-related pain, you could still have other damage or other health issues going on. We never want to assume it is always hemophilia-related pain. Additional information is always helpful.
You may be asked to keep a journal of your pain, or complete pain logs. This may seem like a waste of time, but speaking from a provider’s point of view, I find them very helpful. A pain log helps me with a visual trend in the plan of pain management. If you have to discuss your current plan of care after 1 month of treatment, it might be hard to remember how everything worked for you.
Also, keep in mind that even though you may have a plan for pain management that works for you today, it will need constant reassessment. Your life and health issues may change, requiring an adjustment in your overall plan of care from time to time.Frequently, I have had patients tell me that their pain management plan is not working, yet when we review the journal together, we find that there was some success to the plan, but we might just have to tweak it a bit. Also, by taking the time to document what is going on with you, you demonstrate a level of commitment to working with your provider. It doesn’t have to mean that you have to keep records forever, just when needed.
Development of a good pain management program requires a team effort from you and your provider. It may also involve others: your family, your significant other, and maybe other members of your hemophilia comprehensive care team. Pain can involve your whole being. If you are stressed or anxious, your pain experience can be intensified. Living with daily pain can be exhausting and leave you feeling depressed. These emotions can be normal. Acknowledge them and get help to manage them. Managing these other feelings can help you better manage your pain and help you be in control.
If you feel that your hemophilia treatment center (HTC) can’t get a good handle on your pain and manage it in the way that it is needed, get additional help. Seek out a pain clinic or pain management team-both experts on pain management. Just because you have hemophilia doesn’t mean you have to live with the pain that may go with it. Your hemophilia treatment center can work with other specialists as a team to help improve your care.
|
Pain Checklist for Your HTC Visit: |
|
Use words to describe your pain |
|
Point to where the pain is located |
|
Does the pain stay in the same place or move around? |
|
Describe your level of pain |
|
Make a list of which treatments have worked, and which have not worked for you |
|
Write down what activities make the pain better or worse |
|
List a pain goal you have in mind |
|
Be prepared, knowing that it may take time to find a pain program that works best for you |
|
Bring this list with you |
|
Be Patient |
Angela Lambing has been a nurse practitioner for the past 21 years, and has been working as the hemophilia nurse coordinator at Henry Ford Health system for the past 11 years. Her passions in hemophilia care are focusing on the aging issues in hemophilia and pain. She has participated in research, lectured, and authored many articles related to the hemophilia pain experience.10. Be patient



