
Let’s talk about losing a child. I know, not a feel-good topic, but one I’m living with right now.
The reason I blog, the reason I know why I even know about my own bleeding disorder is because I had a son. I say “had” because he died on Jan. 1, 2021. His name was Max, a lot of you knew him, some of your kids knew him and many of you didn’t.
Max was born in 1992, at the end of the HIV/hepatitis/hemophilia Holocaust age. When he was first born, he was tested every six months for HIV because, although his factor was “probably safe,” no one really knew for sure. Prophylaxis treatment wasn’t a “thing” until he was about 5 years old, but by that time, he already had damage in his ankles and hips. His first major hip bleed happened when he was just over a year old. He was given small doses of Percocet because that was what pain management was then. As a mom, I simply wanted my baby not to hurt.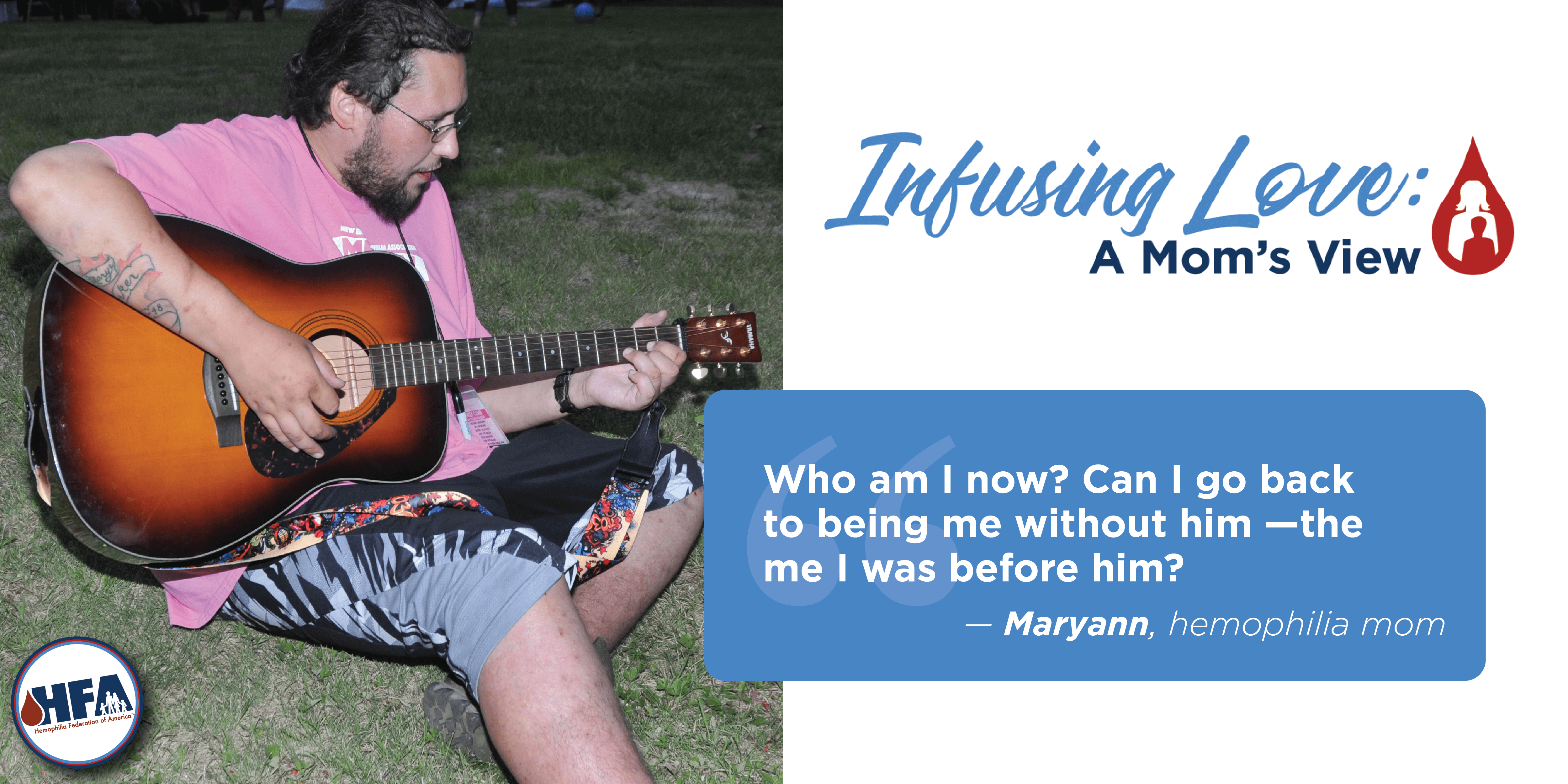 In elementary school he tried to play team basketball, but his left ankle was already damaged, so he had a rolling gate that didn’t allow for running well. Although he was the tallest person in his class, he couldn’t run – that’s not good on a basketball court. After a few tries, he decided he didn’t like the pain it caused, so he stopped.
In elementary school he tried to play team basketball, but his left ankle was already damaged, so he had a rolling gate that didn’t allow for running well. Although he was the tallest person in his class, he couldn’t run – that’s not good on a basketball court. After a few tries, he decided he didn’t like the pain it caused, so he stopped.
He bled, a lot, so much that he had tests for inhibitors. He simply had a very short half-life. When he was 9 years old, his PCP gave him a prescription for morphine. I need to say, it wasn’t the hemophilia treatment center – they didn’t want him to have it. By the time he was 16, the dose doubled to twice a day with Dilaudid for breakthrough bleeds.
In those days, going to any emergency room meant the doctor would look up hemophilia and see pain as a symptom so it was easy to leave with a prescription for opiates. I know this, because we had been in ERs from Chicago to Georgetown. Each time, followed by a visit to the local pharmacy. Camp week almost always included an HTC or ER visit because a week of walking on uneven ground and making sure kids don’t get hurt is stressful on an already taxed body.
He was never able to run, and he was addicted to pain medication by the time he was 11 years old. At 19 he had his left ankle fused; he was told from the time he was 16 he’d need a hip replacement one day. By the age of 15 he faced addiction as well as hemophilia.
When he was going in for his ankle surgery, he turned to me and said, “but I’m only 19, mom. Is this what the rest of my life will be?” His whole life was one lived in pain. I don’t think a lot of people knew that about his pain. I know it was easy for me to forget or deny because what parent who loves their child wants to live with that?
Max had 28 years of life. He lived through losing people to HIV, he lived through learning to self-infuse, caring for his grandmother, teaching younger kids to infuse, CT scans, MRIs, several surgeries, and pain. Always pain. He also saw and did things many people never get to do. He did stay clean for several months. He was in a sober living house at the end. He had just had all his teeth pulled the day before he died, meaning he was in the hospital at the treatment center the night before. Like the good mom-detective I am, I followed the circumstances and I choose to believe he’d simply had enough – enough pain, enough battling addiction, enough knowing his whole life was going to be a repeat of the first 28 years. Even the day before he died, he had the chance to live, to stay with someone who cared and didn’t want him to leave. He chose to go to a place that wasn’t safe.
I find people often want reassurance in times like this, they want to be comforted. That’s not my responsibility. I know I did what I could. I am confident in that. I gave him experiences, travels and people who loved him. I loved him enough that he knew it, above all else. Now I have pictures, a bunch of ashes and memories.
Writer Joan Didion talks about grief in her book “The Year of Magical Thinking.” She talks about the expectation of grief – the crazy feelings. She talks about letting the picture be just that, a picture. At some point we have to let them go, let them be dead. I am letting him go, I am having the crazy feelings, I am living.
I don’t know what life would have been like without hemophilia. When he was diagnosed, we lived with it because there was no other way to live. It became our normal. It just was. It has been so much of who we both became for over 28 years. Who am I now? Can I go back to being me without him, the me I was before him? Only time will show me who this is.
I know that the new treatments mean a lot of kids don’t bleed these days. I worry what will happen when they get old enough to have to have their own insurance and they can’t get the extended life products or injections. What happens when your first bleed happens in your 20s? Then what? Does genetic cure carry on to future generations or is hemophilia going to wait in the background? There’s a saying recovery from addiction, “my disease is waiting for me, it’s doing pushups so it’ll be stronger when it can reassert itself.” Is a “cure” for hemophilia going to be like that? Doing pushups, getting stronger, until it can rear its head again in future generations?
I miss my son. I was his sole parent from the time he was a toddler. We grew up together with his bleeding disorder. We shared jokes, sorrows, achievements and failures. In hindsight I wonder if living with pain might have kept him alive. I guess I’ll never know. Years ago, when Max was a baby, a young man on a panel was asked what to do when a child bleeds, he said “let them bleed.” What I do know is when a parent faces their child being in pain, I want to say to that parent; “let them hurt.”
Maryann is formerly of New Hampshire. Her son, Max, who had hemophilia, died in 2021.
*Note: “Infusing Love: A Mom’s View,” is a blog collection of personal opinions and a representation of individuals experiences. While extensive efforts are made to ensure accuracy of the content, the blog entries do not represent HFA or its Board of Directors. The blog is also not intended to be construed as medical advice or the official opinion/position of HFA, its staff, or its Board of Directors. Readers are strongly encouraged to discuss their own medical treatment with their healthcare provider.
Learn more about opioid dependency
Learn more about managing pain



